Alzheimer’s Care for Seniors: How ReComune Makes a Difference?
Alzheimer’s disease is one of the most prevalent and challenging neurological conditions affecting seniors today.
Updated on: 26 Jan 2026

Loneliness in seniors is far more dangerous than simple sadness it dramatically raises the risk of heart disease, stroke, dementia, and even premature death (JSTOR). This blog enlightens the cutting-edge science, overlooked warning signs, and practical, evidence-based ways families and caregivers can protect their aging loved ones. Loneliness is dismissed as a harmless emotion something we think can be fixed with a quick call or a passing smile. But for older adults, chronic loneliness is a silent epidemic and a severe public-health crisis that quietly damages the body, erodes the mind, and shortens life expectancy.
Groundbreaking research proves that social disconnection doesn’t just weigh on the spirit; it rewires the brain, weakens the immune system, strains the heart and blood vessels, and accelerates cognitive decline. Experts now compare the health toll of loneliness to smoking 15 cigarettes a day or living with obesity (University of New Hampshire).
Nearly one in three middle-aged and older Americans report feeling lonely, a staggering figure that continues to rise as the U.S. population ages. Without timely intervention, millions more risk suffering not only emotionally but also physically.

Loneliness is the subjective experience of social disconnection very different from simply living alone. This invisible burden sets off a cascade of biological stress responses cortisol (the stress hormone) surges, blood pressure climbs, inflammation intensifies, and immune defenses weaken. Over time, these shifts accelerate chronic illnesses, frailty, and neurodegenerative decline (National Institutes of Health)
Loneliness is not just emotional discomfort it is a neurological hazard. Prolonged stress elevates cortisol and inflammatory markers, which gradually damage neurons and shrink brain regions tied to memory, focus, and decision-making. Large pooled analyses, including NIA-funded research, confirm that lonely individuals have significantly higher odds of developing dementia even when depression and other factors are accounted for. This makes loneliness an independent risk factor for cognitive decline (National Institute on Aging).
Caregivers should watch for early brain signals:
Recognizing these early and voicing them to a healthcare provider can profoundly change outcomes. In brain health, early detection is transformative.
Loneliness exerts chronic strain on the cardiovascular system. Research links it to high blood pressure, more hospitalizations, poorer heart-failure outcomes, and elevated risk of heart attacks and strokes.
Meta-analyses show:
For seniors with existing heart conditions, loneliness predicts worse survival rates and more frequent emergency visits.
Why this matters: Heart disease and stroke remain the leading causes of death and disability in older adults. Tackling social disconnection is as critical as managing blood pressure or cholesterol.
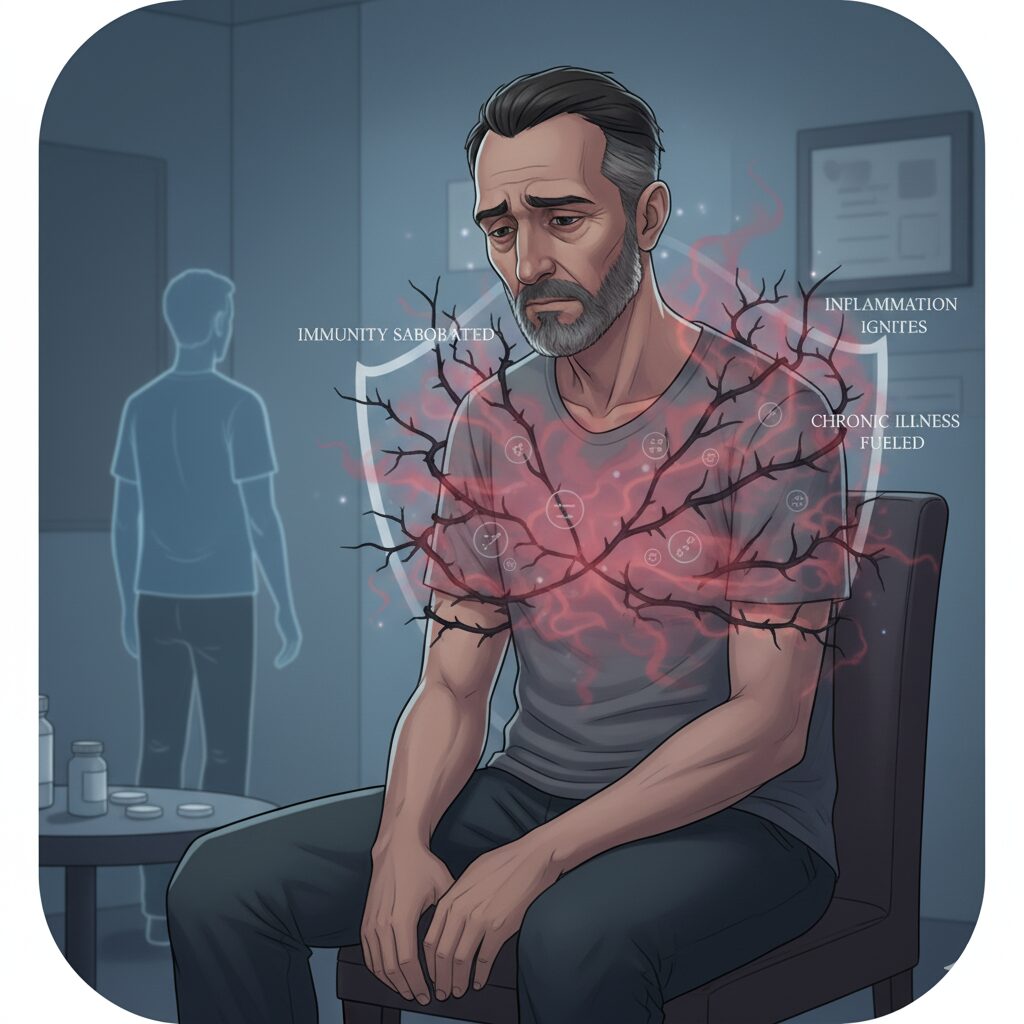
Chronic loneliness does more than hurt feelings it weakens immunity and amplifies systemic inflammation. Studies link it to:
Lonely older adults respond less effectively to vaccines and are more vulnerable to infections. Over time, this cascade magnifies chronic conditions and reduces life expectancy by 3–5 years.
Global data now recognize loneliness as a worldwide public health threat, linked to over 871,000 deaths annually, with effects comparable to heavy smoking (World Health Organization).
While loneliness can strike anyone, some groups of seniors are particularly vulnerable:
Socioeconomic disparities also play a role: seniors with lower incomes report much higher loneliness rates (AARP).

The good news: loneliness is reversible. Even small, consistent steps can improve health outcomes and restore joy. Research shows that meaningful connections lower stress hormones, improve immunity, and strengthen both brain and heart health.
Here are five high-impact strategies families and caregivers can adopt:
Loneliness isn’t solved by random check-ins — it thrives on intentional, heartfelt connections. Instead of quick calls, ask deeper questions: “What made you smile this week?” Studies show that quality matters more than quantity: even weekly 30-minute visits reduce perceived isolation.
For times when loved ones can’t always be present, ReComune AI Companionship bridges the gap offering seniors trusted, on-demand conversation, empathy, and emotional support that helps them feel connected between visits.
Technology can be a powerful lifeline — if it’s simple to use. Set up one-touch video calls, voice assistants, or large-button smartphones so seniors can connect without tech anxiety. Pair this with community-based support, such as local senior centers, faith groups, or volunteer visitors, which have been shown to lower depressive symptoms and social withdrawal in older adults (National Institute of Health).
Feeling needed is one of the strongest buffers against loneliness. Encourage seniors to volunteer, mentor, or even care for a pet. A study published in Aging & Mental Health found that older adults who engaged in purposeful activities reported higher life satisfaction and lower loneliness scores (Aging & Mental Health, 2019). Purpose restores identity, builds natural social contact, and protects mental health.
Often, it’s not unwillingness but practical barriers that keep older adults isolated. Untreated hearing or vision loss can drastically limit social participation, while lack of transportation cuts off access to community life. By addressing sensory health and arranging support such as rideshare services, community shuttles, or volunteer drivers, families can dramatically reopen the door to connection (CCAM-TAC).
Loneliness is not just emotional — it’s clinical. Ask healthcare providers to include loneliness screening during wellness visits, and request referrals to social prescribing programs or counseling services. Since depression and loneliness often overlap, addressing underlying mood disorders can reignite the desire for social contact and reduce health risks (CDC).
Small rituals also matter: sharing a meal, swapping photos, or co-reading a book can create daily micro-moments of belonging that strengthen connection.
Approach conversations with warmth and curiosity. Use “I” statements (“I miss our talks”), normalize the feeling (“Many people struggle with loneliness as they get older”), and offer specific help (“Would you like me to come by Tuesdays?”). Avoid framing loneliness as a character flaw it’s a social condition that needs practical solutions.
If loneliness is paired with persistent sadness, hopelessness, sleep or appetite changes, suicidal thoughts, or rapid cognitive decline, it’s important to contact a healthcare provider promptly. Clinicians can assess for depression, cognitive impairment, and safety risks and connect older adults to community services, mental health care, or social prescribing programs (National Institute on Aging).
Loneliness doesn’t have to be a lifelong affliction it is reversible, and emotional healing is possible at every stage of life. Compelling research demonstrates that cultivating resilient social connections, diminishing chronic isolation, and addressing co-occurring mental or physical conditions can drastically reduce cardiovascular risks, cognitive decline, and overall mortality while elevating vitality, longevity, and happiness. For families and caregivers, even seemingly modest gestures a heartfelt phone call, a consistent weekly visit, or providing reliable transportation function as transformative medicine for the heart, mind, and soul.